Postoperative Pancreatic Fistula Following Duct To Mucosa Pancreaticojejunostomy After 100 Consecutive Whipple’s Surgery
DOI:
https://doi.org/10.3126/njc.v8i1.68233Keywords:
Pancreaticoduodenectomy, postoperative pancreatic fistula, Whipple’s surgery, POPFAbstract
Background: Postoperative pancreatic fistula (POPF) remains a concerning complication following pancreaticojejunostomy (PJ). Its incidence can be as high as 20%, with identified risk factors including soft gland texture, small main pancreatic duct (MPD) diameter, pancreatic pathology, and significant intraoperative blood loss. Our primary objective is to determine the incidence of POPF and assess its associated risk factors by consistently applying a uniform surgical technique and utilizing uniform suturing materials.
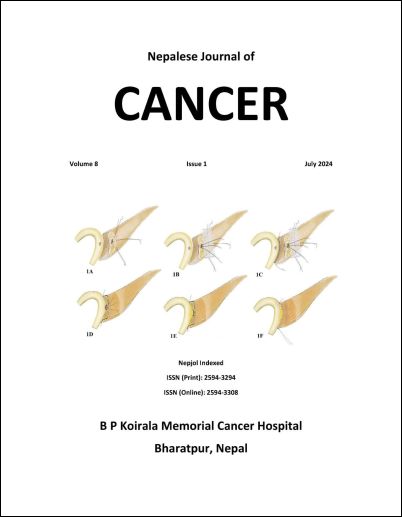
Methods: Our study included patients who underwent PJ following pancreaticoduodenectomy at our center using a consistent duct-to-mucosa technique and the same suturing material, PDS 5-0. Data from 100 consecutive patients were collected and entered into the Statistical Package for the Social Sciences (SPSS 26) for analysis of postoperative pancreatic fistula (POPF).
Results: Among the 100 patients, the incidence of clinically relevant POPF was 5%. Factors such as gland texture and main pancreatic duct (MPD) diameter did not demonstrate any statistically significant correlation with POPF, however the frequency of POPF was notably high in cases with an MPD diameter of less than 3 mm. Mortality following clinically relevant POPF was substantial, reaching 4%, and this association was statistically significant (p < 0.001).
Conclusion: POPF represents a severe complication associated with statistically significant mortality. Employing a uniform standard duct-to-mucosa anastomotic technique along with consistent use of suturing material is imperative to mitigate bias and minimize the risk of POPF.
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Nepalese Journal of Cancer

This work is licensed under a Creative Commons Attribution 4.0 International License.
This license lets others distribute, remix, tweak, and build upon your work, even commercially, as long as NJC and the authors are acknowledged.
Submission of the manuscript means that the authors agree to assign exclusive copyright to NJC. The aim of NJC is to increase the visibility and ease of use of open access scientific and scholarly articles thereby promoting their increased usage and impact.