Minimal Local Analgesic Dose of Intrathecal Bupivacaine and Ropivacaine in Patients Undergoing Cesarean Section: A Comparative Study
Keywords:
Bupivacaine, Cesarean section, Ropivacaine, Spinal AnesthesiaAbstract
Introduction: Spinal anesthesia is considered a reasonable option for cesarean section. Bupivacaine and ropivacaine have been used as intrathecal drugs alone or in combination with various opioids. Ropivacaine is considered a valid and safe alternative to bupivacaine for intrathecal anesthesia. This study aims to determine the median effective dose (ED50) of intrathecal bupivacaine and ropivacaine for cesarean section and defines this as the minimum local anesthetic dose (MLAD).
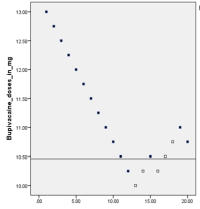
Methods: Forty pregnant women undergoing elective cesarean section were allocated and randomized into two groups. The initial dose was 13mg for both ropivacaine and bupivacaine groups and was increased or decreased of 0.3mg, using the up-down sequential allocation technique. Efficacy was accepted if adequate sensory dermatomal anesthesia to pinprick to T6 was attained within 20 minutes after intrathecal injection and required no supplemental epidural injection for procedure until at least 50 minutes after the intrathecal injection of test drugs. The MLAD for both bupivacaine and ropivacaine was calculated with 95% confidence interval using the formula of Dixon and Massey. Comparison of different variables between the groups was done using t-test with significant p value at < 0.05.
Results: The two groups were comparable in terms of demographic profile and clinical characteristics. The MLAD of ropivacaine and bupivacaine were 11.63 mg (95% CI, 11.5-12.92) and 10.459 mg (95% CI, 10.12-10.87) respectively. The potency ratio between spinal ropivacaine and bupivacaine was 0.89.
Conclusion: Ropivacaine provided clinically surgical anaesthesia of shorter duration without compromising neonatal outcome and can be used as a safe alternative to bupivacaine.
Downloads
Downloads
Published
How to Cite
Issue
Section
License
The Journal of Lumbini Medical College (JLMC) publishes open access articles under the terms of the Creative Commons Attribution(CC BY) License which permits use, distribution and reproduction in any medium, provided the original work is properly cited.JLMC requires an exclusive licence allowing to publish the article in print and online.
The corresponding author should read and agree to the following statement before submission of the manuscript for publication,
License agreement
In submitting an article to Journal of Lumbini Medical College (JLMC) I certify that:
- I am authorized by my co-authors to enter into these arrangements.
- I warrant, on behalf of myself and my co-authors, that:
- the article is original, has not been formally published in any other peer-reviewed journal, is not under consideration by any other journal and does not infringe any existing copyright or any other third party rights;
- I am/we are the sole author(s) of the article and have full authority to enter into this agreement and in granting rights to JLMC are not in breach of any other obligation;
- the article contains nothing that is unlawful, libellous, or which would, if published, constitute a breach of contract or of confidence or of commitment given to secrecy;
- I/we have taken due care to ensure the integrity of the article. To my/our - and currently accepted scientific - knowledge all statements contained in it purporting to be facts are true and any formula or instruction contained in the article will not, if followed accurately, cause any injury, illness or damage to the user.
- I, and all co-authors, agree that the article, if editorially accepted for publication, shall be licensed under the Creative Commons Attribution License 4.0. If the law requires that the article be published in the public domain, I/we will notify JLMC at the time of submission, and in such cases the article shall be released under the Creative Commons 1.0 Public Domain Dedication waiver. For the avoidance of doubt it is stated that sections 1 and 2 of this license agreement shall apply and prevail regardless of whether the article is published under Creative Commons Attribution License 4.0 or the Creative Commons 1.0 Public Domain Dedication waiver.
- I, and all co-authors, agree that, if the article is editorially accepted for publication in JLMC, data included in the article shall be made available under the Creative Commons 1.0 Public Domain Dedication waiver, unless otherwise stated. For the avoidance of doubt it is stated that sections 1, 2, and 3 of this license agreement shall apply and prevail.
Please visit Creative Commons web page for details of the terms.



